RESOURCES FROM CENTRAL DISTRICT HEALTH
By: Jessica Harris
Central District Health is collaborating with Interfaith Sanctuary and Corpus Christi House to honor and remember those in our community affected by drug overdose. The incidence of overdose deaths, particularly those involving opioids, has risen sharply over the past decade. In 2022, Idaho reported 381 drug overdose deaths, with 270 of those linked to opioids and 188 linked to fentanyl. This crisis deeply impacts the community of individuals who use drugs and the people in their lives.
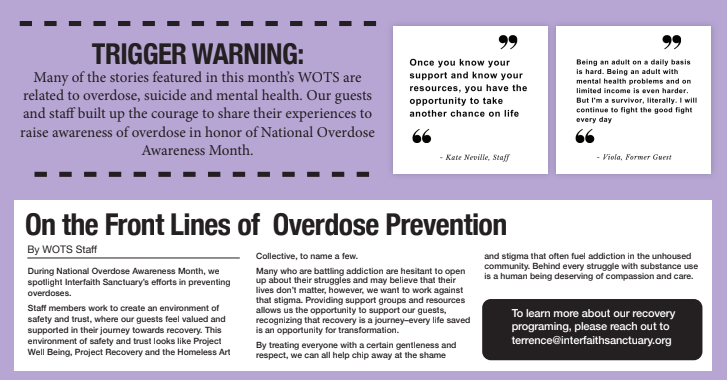
On August 24, 2024, Interfaith Sanctuary will host an Overdose Awareness Event in the Phoenix Room, located at 511 S. Americana Blvd. in Boise, from 1-4 PM. Attendees will have the opportunity to share personal experiences, participate in activities to commemorate and honor those lost, receive training on opioid overdose reversal techniques, and access resources for overdose prevention and response. This event recognizes International Overdose Awareness Day, an annual event on August 31, and is part of the global effort to combat overdose, remember those who have died without stigma, and support those grieving their loss.
Throughout the year, Central District Health offers free overdose prevention and response supplies, including prescription drug locking boxes, Deterra drug deactivation pouches, CPR face shields, naloxone (Narcan), sharps disposal containers, and soon, fentanyl and xylazine testing strips. These resources will be available at the event and online for residents of Ada, Boise, Elmore, and Valley counties. For more information or to access these resources, visit www.cdhhealthcare.com.
Overdoses are preventable, and you can make a difference. For details on training and resources, contact the Drug Overdose Prevention Program at DOPP@cdh.idaho.gov or visit https://cdh.idaho.gov/.
Resources:
There is hope. There is help.
Idaho Crisis and Suicide Hotline: Text/Call 988
Mobile Crisis Response (Region IV): 208-334-0808
Pathways Crisis Center (24/7): 833-527-4747, 7192 Potomac Drive, Boise
FindHelpIdaho.org

ALONE AND AFRAID
By: Julie Loomis
I am sharing why I felt bad enough to attempt to take my life. Facing the unknown can be very difficult. I never felt I would ever fall so far from myself.
My Mom suffered from depression and PTSD. They didn’t treat ptsd back then and even the mental health services were not good. I watched my Mom try to end her life so many times. I never wanted to be that kind of Mom. I didn’t believe in suicide but I think I was fooling myself.
I spent most of my life as a single Mother and my kids came first. I was in two serious relationships, one was actually a marriage. But they never lasted. I worked hard to keep a roof over our heads. My youngest is autistic and has other issues and took a lot to help him. Thank goodness there are better mental health programs.
When Covid hit I caught it a few times and never fully recovered. My other medical issues got worse and suddenly I was so depressed I just went numb. I could barely keep up with my son’s needs and did not take care of my own.
We rented rooms from a man that just needed help cleaning and cooking. I started to feel better but my roommate kept asking for more help. I was not in the right physical or mental place to keep up. My little dog died and we were kicked out. We stayed in our rooms while I desperately tried to find somewhere else to go. The roommate shut the electricity to our rooms and my son couldn’t cope and went to his Dad’s.
I was going to be homeless and with my health issues, I felt like it would kill me. I just wanted to be with my family and my dog. So I got a bottle of wine and felt so alone and scared. I was taking my meds for the night and suddenly thought it was my time to go. I just kept taking pill after pill. I saw my son’s face and realized what I was doing. I stopped and called 911. I was very sleepy and a bit drunk. The emergency service people were very nice.
I ended up in the ER throwing up so I didn’t need my stomach pumped. After 24 hours at the ER I was put on a 10 day suicide hold at a Mental Hospital. I still was numb and didn’t care what happened to me. The doctors treated my depression and felt I was not needing to be committed to a state hospital.
I showed up at Interfaith Sanctuary and being homeless may not be the death sentence and they helped me get back on my feet. The depression is always there. I choose every day to come out of the darkness and choose to keep fighting.

THE BROTHER I NEVER KNEW
By: Karen
In Project Well Being we learn to understand each other and to give each other and ourselves “grace”.
It has not been like that for me. I grew up in a single parent family with Gates, my brother, who was emotionally very disturbed from the time he was three years old on, impossible to understand. My mother took him
to a series of child psychiatrists. He “outsmarted” them all. By never speaking to them he hurt himself immeasurably.
He was sent to a progressive school, and joined the army after graduation. And become a paramedic.
The reality was that he wanted to learn to inject heroin and other drugs more perfectly. He was extremely bright. Technically, he was classified as a genius. And he is an incredibly talented and creative wood worker – a master carpenter.
He adored animals. He would’ve been a fantastic veterinarian.
He decided at some point in his life, after working on the Alaskan pipeline and falling, injuring his radial nerve, to return to Washington state – and became very solitary.
He lived in Port Angeles, Washington. He believed that he was not ok with other humans, and could only relate well to animals so he started raising chocolate labradors. I think he might’ve been happy for sometime.
Then my mother died and for both of us it was a horrible time in our lives, but for my brother it was a defining moment from which he never was able to recover.
He entered himself into a treatment facility in Seattle, Washington and checked himself out in three days.
We never heard from him again and I found out in 2008 that he had died from a heroin overdose and that it was an intentional death.
I’ll never forget how sweetly he played with my daughter when she was a young child of 3 or 4. He adored her and she adored him.
The guilt I carry about him is that I never could get through to him or understand what he was going through.
I remember talking to him a few times about it, but it was impossible to break through the barrier that he had erected around himself.
In this month when we remember those who we’ve known and lost – who have died from suicide, I remember my beautiful brother. I’ll never understand what drove him – what made him tick, and that he’s not here anymore.I can only hope that his spirit is at peace.
The impact on my family cannot be ignored. Gates was a disturbance. I stayed away from him and when he was sent to a “Summerhill” type of school – life became easier. Quieter. My mother and father stopped arguing long distance about “what should be done”.
I had a lot more freedom and my mother had her out -of-town buying trips. I cannot imagine how stressful it was for her. And from then on she and I never discussed my brother in depth.
When she was diagnosed with cancer and we were living in Norway my daughter and I had to return to the US to care for her. My brother begged me to do it.
When he finally came to stay with her he had a gun. I was keeping track of all financial things and I found him on her patio with papers scattered all over – and his gun on the table. He was threatening me with it. I was terrified and called my father who came to oversee how things were to proceed from there. There were lawsuits initiated by Gates because I was the executor of my mother’s estate – over the sale of her home – it was horrible. And then he returned to Washington state.
It wasn’t until 13 years later that I learned of his suicide. In and out of my life, my mother’s and then the final time. A troubled soul lost for good. A brother I could never know.

MY INTENTIONAL OVERDOSE
By: Viola Crowley
***Trigger Warning – Self Harm and Suicide***
I’ve been on mental health meds since I was 22. My first hospitalization was at 22 as well. Been in and out of hospitals from 22 to 31. I used to cut as well and quit in 2009. In November 2008, I was sexually assaulted and told my therapist. We talked about the assault and my fear of telling my husband about it, for fear he would blame me. She asked me to write a pros and cons list for telling him. He found my list before I could go back to therapy and he flipped out. I felt betrayed because he rummaged through my things. Felt scared about what was gonna happen to our relationship. Felt hopeless that I was in another relationship that left me fearful. I felt desperate to end these feelings. I had just filled all my prescriptions. So I locked myself in the bathroom with a cup of water and a 3 month supply of blood pressure meds. I sat in front of the tub and took handful after handful of pills until they were gone. I stayed there on the floor until I felt drowsy and got tired of hearing him pound on the door, begging me to come out. I went out and laid down on the bed to go to sleep. He figured out that something was wrong but didn’t know exactly what. He kept asking me “What did you do?”. He tried his best to keep me awake. You see, I made him promise to never have me locked up like my ex did. So he tried his best to keep that promise by throwing water in my face and flicking a lighter close to my feet to keep me awake, not knowing that my major organs were shutting down. After sleeping for several hours because he fell asleep as well, I woke up and realized I was in trouble medically. I rolled over and dialed 911. I vaguely remember pounding on the door. I do not remember answering the door or being in the ambulance or in the trauma room at the ER. I coded 7 times in 4.5 hours. The last time I coded, the doctors were ready to call time of death. My husband flipped out and begged them not to give up. Begged them that if I kept fighting they needed to keep fighting for me. After the 7th code, they stabilized me enough to send me to ICU and put me in a medically induced coma so my body could heal. I was in heart failure, liver failure, kidney failure and had a collapsed lung. I vaguely recall how they tried to wake me up after 5 days but my body wasn’t ready. My other lung collapsed and I coded again. So they intubated me again and put me back in a medically induced coma. Day 9, they brought me back out of the coma. After they took me off the ventilator, I took a call from my sister and I vaguely remember telling her that my husband tried to kill me. After they transferred me upstairs to the psychiatric unit, my psychologist explained that between my altered state and my fear, I believed that what he was doing to keep me awake was him trying to kill me. I really worked the program and decided that I never wanted to feel that way again. I really didn’t want to die. I made a promise to myself to always take my meds and talk to professionals about my symptoms, as to keep them in check. The only lasting effect of that trauma is my TBI (traumatic brain injury) from lack of oxygen which is the reason for my sh**** memory. I tell my story in hopes that it might help someone else and to remind myself why I work so hard every day to keep my head above water. My next step is to get a tattoo across my forearm to cover my scars from cutting. I want to get the word “Live” with a semicolon for the “I” as soon as I get the money. Ugh. Being an adult on a daily basis is hard. Being an adult with mental health problems and on limited income is even harder. But I’m a survivor, literally. I will continue to fight the good fight every day.
OVERDOSE AWARENESS
By: Terrence Sharrer- Interfaith Sanctuary Project Recovery Director
The first time I overdosed. I was overwhelmed with fear and shame. I felt like I lost control, and that my addiction had taken over my life. But even after that experience, I continued to put myself in danger, continuing to use drugs despite the risks. It was like I was stuck in a cycle of insanity, unable to break free from the grip of addiction.
The battle against addiction is a relentless one. Despite my own overdoses and seeing others suffer and die, I continued to use drugs. That’s the power of addiction-it makes you do things that don’t make sense, even when you know the dangers. It’s like being trapped in a never ending cycle with your mind constantly at war with itself. This mental agony is where hope goes to die. Witnessing others lose their lives to overdoses is a tragic and sobering experience.I have lost loved ones and friends including my nephew to this devastating crisis. He had been clean and sober a year working on his program. He had a bad day and scored some heroin that was laced with fentanyl. His body had no tolerance and he died in his bathroom while his five year old son played in the living room. I have also seen guests at our shelter suffer the same fate. It is tragic and heartbreaking and made me realize just how much more needs to be done to support and protect those struggling with addiction.
Narcan training can be a valuable tool in the fight against overdoses.It can empower people to take action when they see someone in crisis, potentially saving a life. I have seen the miracle of narcan bring people back from the brink of death. Unfortunately not enough people have access to this training. There is a need to make it more widely available and accessible. By doing so, we can better equip individuals and communities to respond to overdoses and prevent more tragedies. It is a small but important step in addressing the overdose crisis and reducing the stigma surrounding addiction.
Reducing the stigma surrounding addiction is essential if we are going to effectively tackle the overdose crisis. For too long addiction has been seen as a personal failing or a sign of weakness. This type of thinking only serves to isolate and shame those struggling with addiction, making it harder to seek help.
Instead we need to treat addiction as the public health crisis it is, and provide support and resources for those in need. Only then can we begin to address the underlying causes of addiction and work towards reducing the number of overdoses.
There is also a urgent need for more long-term treatment options and programs. Right now many people struggling with addiction are unable to access the support they need to recover. There often long waiting list for treatments centers and not enough affordable options available.This needs to change if we want to effectively address the overdose crisis. We need to invest in more treatment facilities, support programs, and harm reduction initiatives to help people access the help they need and reduce the number of overdoses.
Ultimately, I’m tired of attending funerals and vigils for those lost to overdoses. It is a devastating and exhausting cycle, one that takes a toll on individuals, families, and communities. But I’m hopeful that by raising awareness, reducing stigma, and increasing access to resources, we can work towards a future where fewer lives are lost to overdoses. Especially in our Interfaith community. It won’t be easy, but it is a fight worth having.